Rethinking Depression: Beyond the Chemical Imbalance
In recent years, the long-accepted monoamine theory of depression—which suggests that depression is caused by a deficiency in neurotransmitters like serotonin, dopamine, and norepinephrine—has come under scrutiny. Emerging research shows that many individuals with depression actually have adequate serotonin levels, making it difficult to prove a straightforward neurotransmitter deficiency.
While antidepressants remain effective for many clients, our understanding of how they work is evolving. Rather than simply replenishing depleted neurotransmitters, antidepressants may function by enhancing neuroplasticity and improving the way these brain chemicals are released and transmitted.
The Rise of Microbiota Research
At the same time, microbiologists like Dr. Justin Sonnenburg at Stanford University have been making fascinating discoveries about the gut microbiota. We now understand that the human body is composed of approximately 43% human cells and 57% microbial cells. In fact, 10 to 100 trillion microbes—representing thousands of species—reside in our gastrointestinal tract. This thriving community of microbes, known as the gut microbiota, plays a crucial role in regulating our immune system, metabolism, and even our mental health.
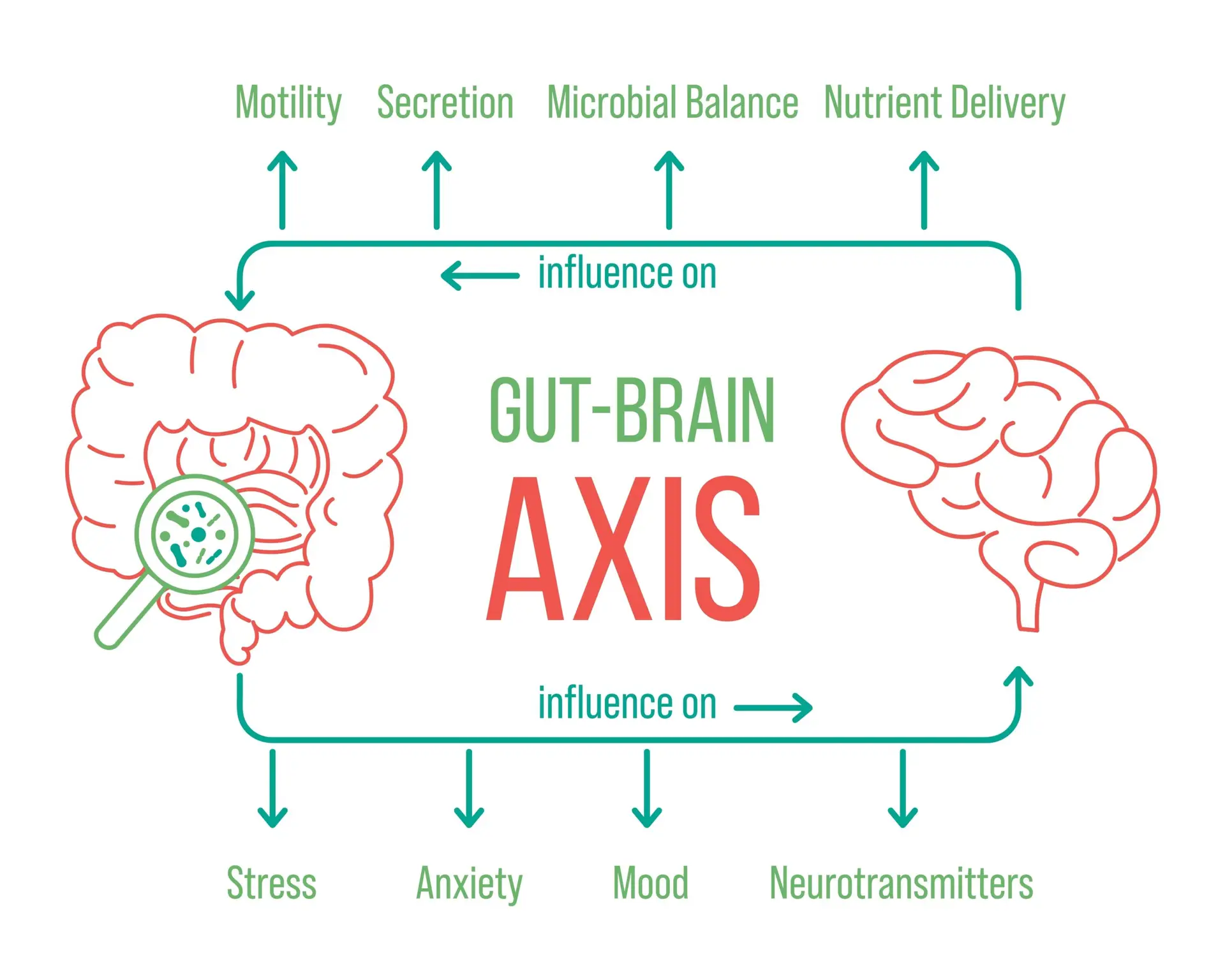
The Gut-Brain Axis: A Two-Way Street
This research highlights the importance of the gut-brain axis—a communication network linking the gut and brain. As someone trained in psychosomatic medicine, I find this especially helpful in working with clients. Many are already familiar with the benefits of good sleep hygiene and exercise for mood regulation. But now, more clients are asking about diet—particularly how highly processed foods can harm the balance of their gut microbiota.
Why Fiber Matters: Feeding Your Gut to Protect Your Mind
Diet is a major factor in determining which microbes thrive in the gut. One of the most important components for gut health is microbiota-accessible carbohydrates (MACs), which are found primarily in dietary fiber. These carbohydrates are the preferred fuel source for beneficial gut bacteria. When our diets lack fiber, these microbes look elsewhere for sustenance—often turning to the body’s own mucus lining for food.
This can weaken the protective gut barrier, allowing toxins to enter the bloodstream and triggering inflammation. A helpful way to think about it: when we don’t feed our gut microbes properly, they start eating away at the foundation of our health. This process has been linked to an increase in inflammatory markers such as interleukin-6 (IL-6) and C-reactive protein (CRP), which are commonly elevated in clients with mood disorders.
Empowering Clients Through Lifestyle Education
Clients living with depression or anxiety often feel a loss of control over their mental health, which can be disheartening—especially when medication is the only option presented. But when we talk about mental health in the context of diet, sleep, and lifestyle choices, we empower clients to take an active role in their healing. This is at the heart of client-centered treatment.
Even small changes—like increasing fiber intake or choosing whole foods over processed ones—can foster a sense of agency and positively impact mood, cognition, and overall well-being.
A Holistic Path Forward
Healing doesn’t come from one source alone—it’s cultivated through daily choices, compassionate care, and a growing understanding of how deeply connected our minds and bodies truly are.